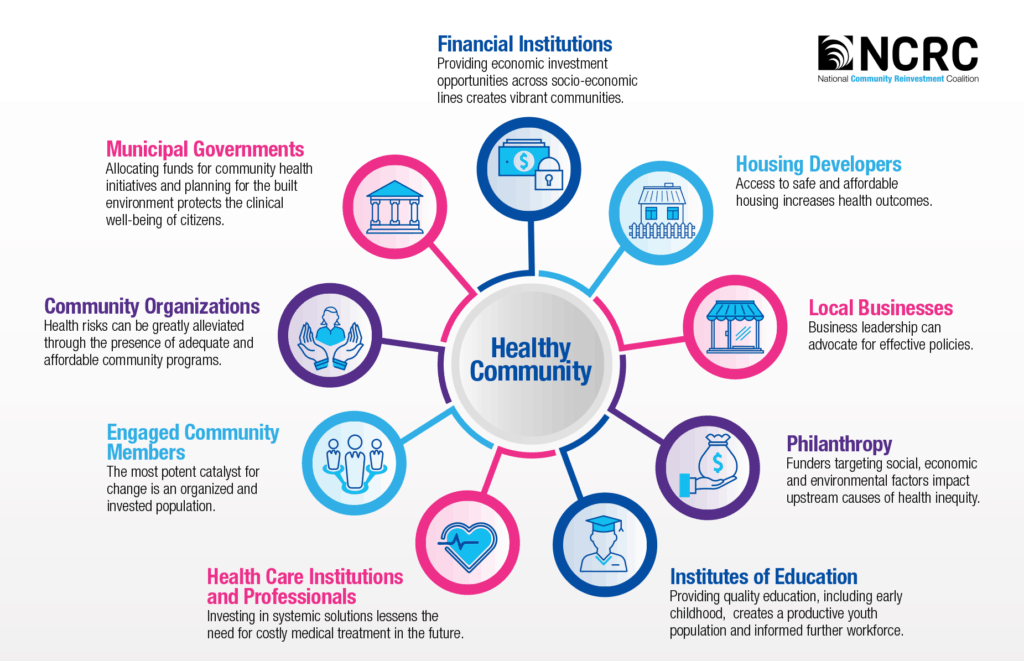
NCRC’s mission is to create opportunities for individuals to build wealth. But building wealth isn’t just about saving money or improving access to lending. Economic wellbeing is intrinsically tied to social, physical and mental health, and financial instability has a direct ramification on a person’s health. A lack of stable housing in a safe environment can increase the risk of disease, and determine access to treatment.
This relationship, known as the Social Determinants of Health, is defined by the Centers for Disease Control and Prevention (CDC) as “conditions in the environments in which people are born, live, learn, work, play, worship and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” The CDC specifies that conditions that influence wellbeing are largely dependent on where a person lives. As an increasing number of American cities report double-digit life expectancy gaps for different neighborhoods within their borders, health experts have begun to consider zip-codes as powerful a health determinant as genetic codes.
Therefore, when discussing the importance of building wealth and securing fair housing, there must be a focus on the health inequalities that prohibit many families from achieving these goals.
In 2018, NCRC partnered with the Center to Advance Community Health and Equity (CACHE), as one of three national organizations spearheading an initiative to pilot the use of Community Benefits Insights (CBI) and related tools to focus diverse assets in communities where health inequities occur. Together, CACHE and NCRC implemented two convenings, one in Wilmington, Delaware, and the other in Baltimore, Maryland. These events were designed to bring senior leaders from health care, municipalities, financial institutions and community development to the table to build common knowledge of trends across health and development sectors, and to explore practical strategies to align resources. The convenings launched a conversation amongst stakeholders about the potential value of ongoing collaboration to reach their shared goals.
Members hone in on health equity
As coverage expands and financial incentives shift, hospitals need to move beyond the delivery of acute care services to improve the health and well-being within our communities. Listening sessions with members and a Healthy Communities Community of Practice convened by NCRC concluded that health care institutions can and should adopt an up-stream care model, focused not only on curative treatment but also on preventative efforts and holistic community solutions.
Diverse stakeholders — many of whom are NCRC member organizations — seek the engagement of health institutions as partners in addressing the social determinants of health, such as housing and food access.
With its focus on increasing wealth and affordable housing in LMI communities, NCRC can facilitate this connection between community development and health. We’re aiming to broaden the role of hospitals in developing and maintaining community health. Nonprofit hospitals are required to provide benefits to their communities in order to maintain their tax-exempt status. However, the vast majority of what hospitals report as community benefit is still in the form of free and discounted clinical services, mostly to treat conditions that could have been prevented.
Utilizing its community organizing power and partnering with invested members and key collaborators in the fields of health, community and financial development, we’re turning next to preventative and systematic healthy community solutions to improve health outcomes for low-income families, individuals and entire communities.
Karen Kali is the program manager for Special Initiatives at NCRC
Emily Schreer was a summer intern at NCRC